Corneal Transplants
The cornea is the transparent tissue in the front of the eye, sort of like the windshield of your car. Certain diseases, genetic or acquired, and trauma can lead to the loss of clarity of the cornea. In these cases, the cornea needs to replaced with a corneal transplant. Most conditions requiring a corneal transplant only affect certain layers of the cornea. But for over 100 years, the only way to replace any layer was to replace the entire cornea, a procedure known as a penetrating keratoplasty (PKP), which permanently weakens the eye.
However, for the past 10 year, patients in the North Central Florida area in need of a corneal transplant in order to restore their vision have had another option thanks to the ophthalmologists at Ocala Eye. Endothelial keratoplasty (EK) allows for the partial replacement of only the diseased layers without affecting the strength of the eye and usually requiring no sutures. The two most common EK procedures we perform today are DSAEK (pronounced dee-sek), Descemet’s Stripping Automated Endothelial Keratoplasty, and the newer version known as DMEK (Descemet’s Membrane Endothelial Keratoplasty). Both forms of EK transplantation are associated with quicker visual recovery, a smaller incision, and much less astigmatism than the standard corneal transplant technique (PKP). Both DSAEK and DMEK were first introduced in Central Florida by Ocala Eye.
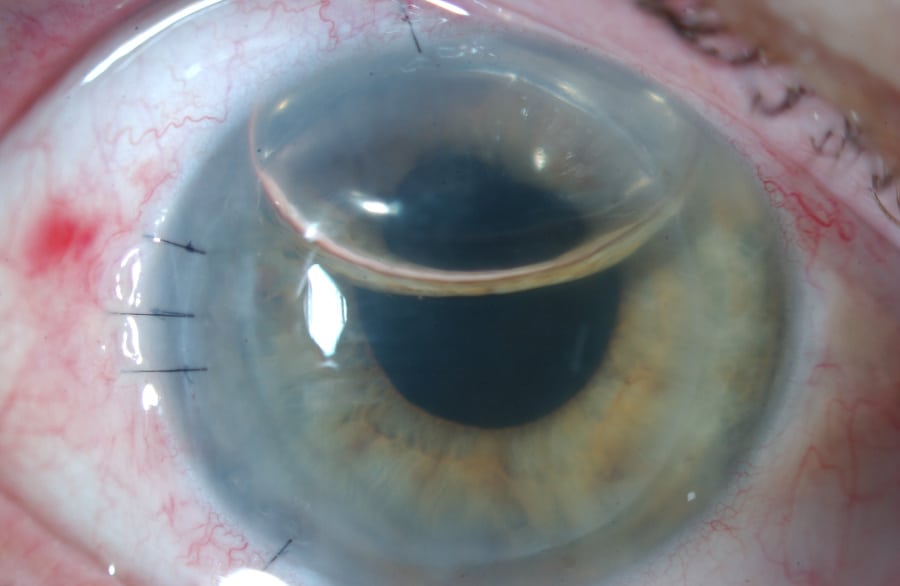
EK on Post-op Day 1 – notice the air bubble used to hold the transplant graft in place instead of sutures (which are present only in the wound itself to keep the air bubble inside the eye)
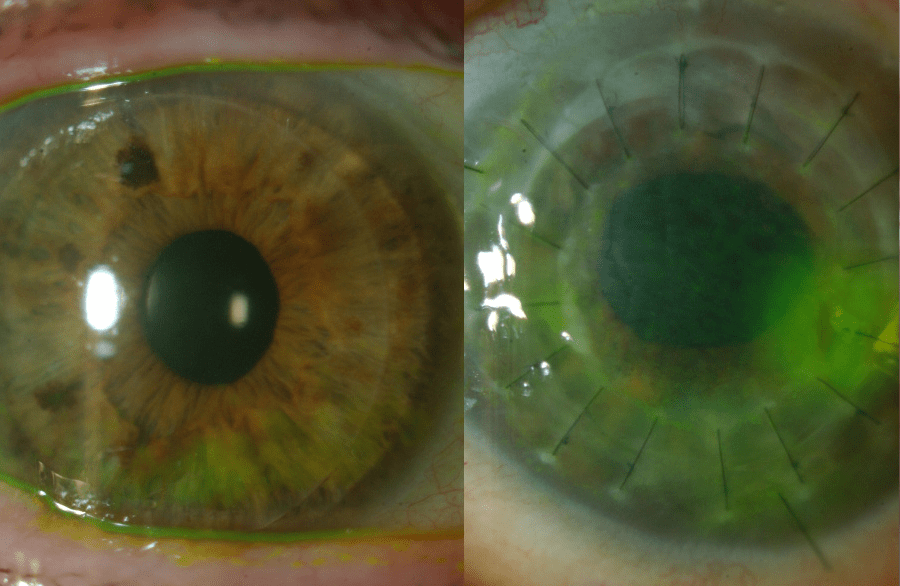
EK vs PKP – A DSAEK sutureless transplant (left) and a PKP or penetrating keratoplasty (right) – requiring multiple sutures 360 degrees around – in the same patient. While the right eye was seeing well within two weeks, the left eye took 6-8 months.
DID YOU KNOW?
After EK (DMEK & DSAEK), the vision clears much faster than the full thickness corneal transplant operation and you can return to many of your normal activities within two weeks with the exception of swimming.
Standard Cornea Transplant Method (PKP)
PKP (penetrating keratoplasty) has been the standard of care for many years and most physicians are very familiar with the postoperative care. It provides excellent vision with the appropriate glasses or contact lenses in most cases. It does require frequent visits to the doctor to measure the cornea, prescribe glasses, and take care of the stitches.
The cornea is a transparent dome on the front of the eye. Corneal edema (swelling) produces decreased vision due to loss of transparency of this normally clear tissue. The swelling arises from a loss of endothelium, a thin layer of cells found on the back surface of the cornea. These cells are not capable of dividing or repairing themselves. The only treatment for visually significant corneal swelling is to replace these cells.
Until recently, the only way to replace endothelial cells was to replace the entire cornea with a donor cornea using a penetrating keratoplasty (PKP). Unfortunately the wound can take years to heal so the new cornea is sutured in place with very fine stitches left in place for a long time to maintain strength and stability. After the operation, it usually takes several months to years to obtain your best vision. It is very difficult to predict the final curvature of the cornea; so after surgery, glasses or contact lenses are required in the majority of cases. If the stitches break, there may be a feeling like having sand in the eye, and removal of the stitches may change the curvature of the cornea requiring new glasses. In addition, the broken stitches may produce a corneal infection requiring the use of antibiotics to treat the infection and can rarely lead to graft failure.
PKP procedures are less commonly performed today but are still necessary if all of the layers of the cornea are affected such as scarring, infection or trauma. In these cases, partial transplantation will not restore the clarity of the cornea.
The EK (DMEK & DSAEK) Advantage
In the mid-2000’s, corneal transplantation surgery was revolutionized with the introduction of endothelial keratoplasty – DSAEK in 2006 and DMEK in 2009 – a new procedure that replaces the endothelial cells without the need for a full thickness replacement of the cornea. In both DMEK (Descemet’s Membrane Endothelial Keratoplasty) and DSAEK (Descemet’s Stripping Automated Endothelial Keratoplasty), a very thin piece of donor corneal tissue containing the endothelial cells is inserted through a small incision on the side of the eye. This tissue adheres to the back surface of the original cornea and restores the cornea’s clarity. The donor tissue is held in place with an air bubble in place of sutures.
The advantages of EK are that, since the wound is much smaller, extensive stitching of the cornea is not required, the eye maintains most of its structural integrity and it heals more quickly. Although glasses may still be required after the operation, they may be much thinner as the power of the eye after surgery is much more predictable. In many cases, patients see well without glasses.
The main difference between the two procedures is that the donor tissue in DSAEK is thicker and easier to manipulate (comprised of Descemet’s membrane, endothelium and stromal connective tissue), so this procedure is preferred in eyes with significant clouding of the cornea or with previous glaucoma or retina surgery. In otherwise healthy eyes, DMEK is preferred. It is a technically more difficult procedure as the donor tissue is much thinner, comprised of Descemet’s membrane and endothelial layer only, but because of this the visual recovery is even faster.
The main disadvantage of the EK procedures (DMEK & DSAEK) procedure is that the new donor endothelium is manipulated more directly than in a full thickness corneal transplantation, potentially producing more damage and possibly increasing the risk of graft failure. There is a 5-10% chance that the new tissue will not adhere properly requiring repositioning, or in less than 1% of cases, re-operation. The long-term survival of this tissue has not been fully studied but research suggests the the lifetime risk of rejection is lower than with full-thickness transplants.
In order to make the new tissue stick onto the back of the old cornea, an air bubble is used to fill the front part of the eye. Since air rises, the patient needs to lie face up as much as possible for the three or four days, until the new tissue has a chance to anchor into place. Short breaks are allowed for meals and bathroom breaks. But these first few days are critical in order to ensure that the graft stays in place.
The position of the graft will be checked the day after surgery. In rare cases, it may be necessary to reposition the new tissue by placing a new air bubble. But once the tissue sticks, it remains in place, so the most critical period is the first two weeks.
After the EK (DMEK & DSAEK) Procedure
After EK (DMEK and DSAEK), the vision clears faster than the full thickness corneal transplant operation and you can return to most of your normal activities within two weeks with the exception of swimming. Like full thickness corneal transplantation, eye drops are required for at least a year and often for the rest of your life to prevent graft rejection, where the body recognizes the tissue as being foreign and reacts against it. Fortunately graft rejections are very unusual (less than 10% of cases) and if they do occur, can be treated successfully in the majority of cases with frequent eye drops and occasionally oral medications. The cornea is a privileged site and normally without blood vessels, so powerful immunosuppressive medications such as those associated with heart or kidney transplants are rarely necessary to prevent graft failure.
Ocala Eye is pleased to introduce these new procedures to central Florida and we look forward answering any questions you might have about your corneal condition.
Consult an Ophthalmologist
Ocala Eye’s fellowship-trained ophthalmologists and medical staff are dedicated to helping your vision last a lifetime, which is why we offer comprehensive eye care for adults of all ages. From annual eye exams to advanced procedures like LASIK and cataract surgery, we can help you see your best at any phase of your life.
